Scarless Suturing
Scarless Skin Closure Techniques
Melanesians
have a High Risk for Hypertrophic Scars and Keloids. Therefore, to achieve a scarless closure of any Open Surgical
Wounds, carried out on the Melanesian Skin is a great challenge. Most times, we
choose Minimally Invasive Techniques such as ‘Sclerotherapy’. However, sometimes, it is
absolutely necessary to do an Open Surgical
Excision to remove any lumps or bumps beneath the skin & then manually suture the opened skin edges together.
Requirements
& Guidelines to Achieve Scarless Skin Closure in the Melanesian:
1. Clean/Straight
Incisions/Cuts
2. Hemostasis (Stopping
of Bleeding) Without Much Use of Diathermy Heat or Use a Bipolar Instead
3. Choice &
Size of Suture Materials
4. Choice of
Suturing/Closure Technique
5. Anatomic Location
of Wound (Tension, Sebaceous Glands, Skin Thickness, etc.)
6. Skin Undermining
(tunneling) & Excision of Sebaceous Glands (skin glands that produce
oil/sebum)
7. Contour &
Skin Color (Avoid ‘Dog Ear’, etc.)
8. Consider Closing
Corners First,
Inside/Median Side First then Outside/Lateral Side
9. Consider Scar
Contractures on Joints (Z-Plasties)
10. Good Diet
& Avoid Strenuous Physical Activities, Post Operative
11. Wound Dressing
Methods & Timing
12. Avoid Stitch/Suture
Marks (Timing of Stitch Removal, etc.)
13. Infection Control
(Choice of Antiseptics & Antibiotics)
14. Non-Smoker
(Avoid Active & Passive Smoking)
15. Monitoring/Follow-up
of Scar & Continued Treatments (Pressure Therapy, etc.)
Notes on Multiple Flaps/Corners for Closure Including Multiple W-Plasties:
1. It takes a lot of time plus effort & may be difficult to incise (execute precisely)
2. Small & Multiple corners on flat surfaces are difficult to stitch-up, have poor blood supply & there is high risk for tip necrosis3. We prefer a straight line closure, blending into natural creases & wrinkle lines & simple & single Z-plasties across/over joint surfaces/creases (perpendicular to)
A Case of a Nose Lump (Exostosis/Osteoma or Benign Bony Outgrowths of the Nasal Bone), Excised & the Skin Edges Were Sutured Using our Finest Suturing Technique. Note the skin darkening from excess skin but a tiny straight scar line.
Notes on Multiple Flaps/Corners for Closure Including Multiple W-Plasties:
1. It takes a lot of time plus effort & may be difficult to incise (execute precisely)
2. Small & Multiple corners on flat surfaces are difficult to stitch-up, have poor blood supply & there is high risk for tip necrosis3. We prefer a straight line closure, blending into natural creases & wrinkle lines & simple & single Z-plasties across/over joint surfaces/creases (perpendicular to)
A Case of a Nose Lump (Exostosis/Osteoma or Benign Bony Outgrowths of the Nasal Bone), Excised & the Skin Edges Were Sutured Using our Finest Suturing Technique. Note the skin darkening from excess skin but a tiny straight scar line.
Another case of Naso-Labial Flap, Donor Site Straight Line Closure Technique.
-The flap is attached to the defect & delayed (left attached) for 3-4 weeks.
-This will allow blood vessels to grow in through the contact skin edges
-After that the flap can be safely divided & the part of the skin covering the defect can survive
The blood supply of the Naso-Labial Flap is from the Facial Artery. During the time of harvest, this artery must be included within the flap, otherwise there will be flap necrosis (skin becomes black due to no blood supply).
Achieving Almost a Scarless Healing with a Z-Incision for Open Rhinoplasty. A 'Z' Makes it Easy to Incise and to Close Later on, with Good Healing.
We also apply our technique of scarless skin closure to large defects. See here, our technique of closing a scalp (head) defect and also the harvesting of a Latissimus Dorsi Flap to Reconstruct a Neck Defect & the closure of the donor site defect. We prefer a straight line closure.
Scalp Alopecia (Defect) Using a Single Straight Line Closure.
Estimating the tension of skin closure.
Design (Drawing over scar to be excised) & trimming of surrounding hair.
Undermining, to reduce tension of skin closure.
Skin edge approximation, to check if undermining is enough (reduced tension).
The defect is closed using a one-layered Nylon, running/continuous suturing, locked (a knot is tied) at 4 intervals only.
One week after removal of stitches. Take note of the tiny linear scar.
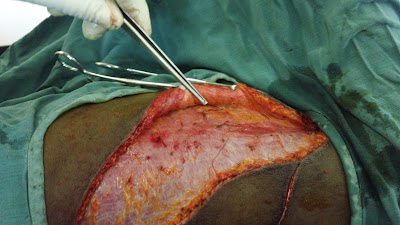
The Harvesting of a Latissimus Dorsi Flap to Cover Defect of the Neck, followed by the closure of a very large donor site defect, using our fine technique. Marking out of the maximum size of skin that can be harvested.
Skin undermining to release/minimize tension.
A very large donor site defect, after complete flap elevation, that needs to be closed.
Partial Donor Site Closure before application of flap, to reconstruct a neck defect.
Appearance of donor site scar after 1 week.
This
is the First Case of Latissimus Dorsi (LD) Flap
Reconstruction Done in PNG by a Local Surgeon, Using
a High Level of Scarless Skin Closure Technique.
Despite
that, there was No Water Running in the Operation Theatre Taps
for Scrubbing (Washing Hands). Rain Water Fetched
in a Plastic Container the Previous Day & Ordinary
Laundry Bar Soap, was provided instead, for Scrubbing
(Washing Hands). Despite that, the Surgery Went
Well and Its Post-Operative Outcome was Superb.
Before Reconstruction of the Neck Defect (Scar Contracture, which was excised totally) using the above harvested Latissimus Dorsi Flap.
After Reconstruction (covering of the excised scar tissue defect, using the latissimus dorsi flap).
Other Methods for Obscuring Scars:
1. Blending Incision/Suture Lines into Natural Crease & Wrinkle Lines
2. Putting Incision/Suture Lines in Non-Visible Areas
Hiding the Scar Within the Naso-labial Natural Crease Line.
This patient underwent Open Intra-Arterial Sclerotherapy for Artherio-Venous Malformation of the Upper Lip. The incision is done to visually locate the main artery (feeder) that feeds blood into the swelling, rather than through a catheter; The Superior Labial Branch of the Facial Artery! The Sclerosants convert the vascular malformation into a lump of scar, which was later excise, through the inner part of the upper lip (obscuring/hiding the scar).
It was found by Taylor, a famous Australian Plastic Surgeon, that somehow Arterio-Venous Malformations form along Choke Zones. Choke Zones are borders of Angiosomes (1 area supplied by a single vessel or arterial branch)
Take note that the scars are successfully hidden along the naso-labial crease and the intra-oral side of the lip. Note almost the scarless final appearance of the incision sites as well as the total shrinkage of the Arterio-Venous Malformation.
The Anatomy of the Facial Artery & its Main Branches.
Arterio-Venous Malformation Explained by Dr. William Mol (Vascular Anomalies Specialist).
*Truncal means more central, large vessel (Artery, Vein or Lymph Vessel)
In our patient above, we noted the absence of the superior labial Arterial Branch on the right side only. We then deduced that the branches from the Superior Labial Artery on the Left side connected directly to the branches of the Superior Labial Vein from the Left Side, Without any Capillary Interposition.
Our techniques of scarless surgery, described here, is scheduled to be published in the New PIH e-Med Journal in November 2017.